No real inspiring lessons here… just a really long (but eventful) update.
TLDR: Click to skip to the bottom if you don’t want all the deets.
In August, my oncologist scheduled me for two more rounds of chemo before my September 19th surgery. That would complete the 12 rounds originally prescribed in January. However, the GI surgeon said she wanted me off chemo for 4 weeks before she operates, and getting two more rounds meant I wouldn’t finish in time.
So I brought this up with the oncologist on July 31st. He said that because I’d only be on low-dose 5FU, it would be okay to finish chemo at 3 weeks prior, instead of 4. I said, “Okay… will you just let my surgeon know this is what you want to do?”
He agreed.
Geeking Out
That next week I spent more time reading medical journals. I had been too overwhelmed to process anything more than a surface-level understanding of my diagnosis until recently, but now I felt more ready to deepen my understanding of cellular biology. So I unearthed my old appointment notes and began to research all the unfamiliar terms so I could more fully grasp the whole picture, while also taking a braver look at my actual prognosis.
The more I studied, the more sobering it became. I realized more and more how rare my case is (particularly because of the mass in my retroperitoneum and my particular combo of DNA mutations), and how much research doesn’t yet exist for how to best treat it. I learned that due to at least one of my mutations, it was unlikely that the cancer would even respond to the chemo.
“In N2 patients TP53 [mutation] was not predictive for an effect of 5FU most likely because there is no effect of 5FU in these advanced patients.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4563117/
Somewhere – I’ve lost the link – I also learned that one of the drugs was only expected to be effective in about 12% of the patients with my condition. At least to date, gratefully, it seems that I’ve been one of the 12%.
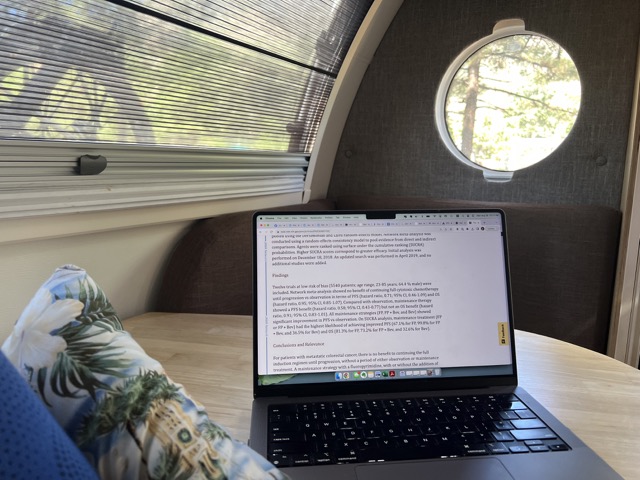
Doing research always raises more questions, but I’ve been enjoying the challenge. It’s like being on a treasure hunt, to identify meaningful questions, and then actually find relevant case studies that answer them. It’s been stretching me and my vocabulary like crazy. Sometimes I’ll start with just one open page, but if I don’t understand a term, I open a new tab to get a definition. Sometimes that leads me to info that contradicts something I already found. So I feel like I have to keep them both open until they’re reconciled.
Oftentimes, it seems they don’t reconcile at all. So then, can I close the tab?? Usually I keep it open in case I need to find it again before I forget what I’m looking for (and why).
Here’s what my desktop looked like while I tried to understand all this stuff. Notice the three layers of open tabs at the top:
Here are some of the conclusions I’ve drawn so far…
Please feel free to skip this next part!
[Start of medical mumbo jumbo]
What follows represents only about 10% of my research. I’m including it here just for my own notes, but maybe it will also give you a sense of how dizzying this has been. Things I wondered:
- Since my TP53 is mutated, is that the only tumor suppressor gene there is? No – I learned there are a lot of different tumor suppressor genes. Tens, if not hundreds. (Another reason why research is overwhelming… there’s a lot of contradictory info out there. Are there 1,000? or are there 30?) Sometimes you have to pay attention to the dates:
The science is always changing as new discoveries are made. Some of the articles I found which appeared to be relevant to my situation were only released in the last few months!
Here were some of my other questions:
- If my sample had the TP53 mutation, does that mean every cell in my body has the mutation? No – I learned that only the cells that divide from that first mutation will also have the mutation.
- Can other genes take up the slack if my TP53 gene isn’t doing its job? Potentially. p51 is a functional and structural homologue of the p53 gene and thus a candidate tumor suppressor gene. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1716054/
- Micronized Zeolite activates p51, which can potentially compensate for faulty p53. https://vimeo.com/800769356 minute 5:38.
- (Yes, I’ve been taking the zeolite, and yes, I signed up to get wholesale. I’ve been running my own sort of personal clinical trial with it. I started in January at the recommendation of a friend, paused during chemo since I wasn’t sure at that point if it would counter the damage we were trying to inflict on my cells or not, and then got back on it again starting last month in prep for surgery. I’ve also been boosting my system with other supplements and am still doing pretty well with my diet changes.)
- However, In contrast with the “ubiquitous” (everywhere) expression of p53, expression of p51 mRNA was found in only a limited number of tissues (not the tissues that matter in my case). https://pubmed.ncbi.nlm.nih.gov/9662378/
- But, the effects of clinoptilolite [zeolite] on cancer cell lines and in tumors both in vivo and in vitro are primarily considered to be caused by the induction of apoptosis and the zeolite’s activation of the p21 tumor suppressor gene. https://cdn.raveretailer.com/A4D99D7E5E/2022/04/GSR_6266de463d8618547271650912342.pdf, https://pubmed.ncbi.nlm.nih.gov/11434724/
- So… good news (maybe)… p21 IS found in colon cancer tissue. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6721478/
- But can the micronized zeolite activate p21 with a faulty p53? Apparently so: “While p21 is strongly induced by p53, resulting in p21’s important impact on cell cycle arrest, high p21 levels can arise also independently of p53.” https://www.nature.com/articles/s41418-022-00988-z.
- Also, “p21 in the absence of p53 is sufficient for the downregulation of p53-repression targets.” https://www.nature.com/articles/onc2013378
[End of medical mumbo jumbo]
Good stuff, but like I said… dizzying.
More About my Prognosis
From the beginning, I’ve told people “my prognosis is good” because that’s what I believed to be true, based on my surface-level understanding of my condition. According to the American Cancer Society, the 5-year relative survival rates for colon cancer are: Localized: 91%; Regional: 72%; Distant: 13%.
I believed mine was Regional, so 72% didn’t seem so bad. Plus, my doctors have always been cheerful and optimistic with me, which I interpreted to mean “optimistic about my prognosis”, but which, in hindsight, may have been merely an expressed optimism about how I would do with the next treatment or procedure.
But getting past the fear that there’s a chance I might not get through this (aka facing my mortality) increased my curiosity around the cellular biology of my diagnosis. As you may have noticed, the more I found, the more questions it raised. And the more I researched, the more dire my situation seemed to feel, particularly when my research centered on retroperitoneal masses.
The amount of information there was to digest was staggering, but I couldn’t stop! I was as fascinated with God’s greatest creation (the human body, imho) as I was with the apparent severity of my condition.
Why not just trust the layman explanations I get from my doctors?
I do think there’s a time and a place to do just that. Like, when I was first getting my diagnosis and it was all I could do to process that much. But now that I’ve been on a lower dose chemo regimen for a few months and regained some of my brain function, I feel a compelling responsibility to learn as much as I can, so I can become my own best advocate. After all, shouldn’t I be at least as invested in finding the right approach for my own case as any doctor, scientist, or researcher would be?
Okay, so now let me catch up on some of the events since my August 3rd update.
Colonoscopy – Friday, August 11, 2023:
This was actually my first colonoscopy ever. I had been too inflamed back in January to have one before my colectomy. I’m telling you what, prep was rough! I learned an important lesson: always start sooner than they recommend, and take the prep drink slower over time so you’re not feeling like throwing it up or stressing out at midnight whether or not it’s going to work in time. I think I’d rather be hungry a little longer going into a colonoscopy than to be up all night wondering if I’m going to have to reschedule and do the prep all over again another time.
Thankfully, the drink wasn’t anything like this:
My prep was just a clear, tasteless powder that I could add to any drink of my choice. The drink itself wasn’t brutal – it was the quantity of liquid I had to get down that made it rough. 64 ounces is a lot, and I worried that I might throw it up before it had a chance to do its job. Next time – I’ll take longer to get it down, and skip a meal or two if it helps me avoid the discomfort of doing the prep at what felt like the last minute.
I think I was finally all cleaned out by 2 or 3am. Check in for the procedure was only a few hours later at 6:45 am. At least everything went off without a hitch and there were no more polyps discovered. Also, best nap in the world. 🙂
During the procedure, the doctor took a biopsy of the Hartmann’s pouch staple line where the PET scan had lit up in June, to verify it was only inflammation. It would be a few weeks before we’d get those results.
Chemo Round 11 – Monday, August 14, 2023:
When we visited with the doctor before my infusion, he said, “This will be your last round before surgery, and we’ll stop the Avastin.”
“So I won’t have another one in two weeks?”
“No, they don’t want you to do that. The surgeon wants you to be off for four weeks.”
That was good news because I was not looking forward to another round, nor was I lovin’ the Avastin. Round 9 with it hadn’t been bad, but Round 10 (with the same dosage) had been rougher than expected. Certain chemo side effects can be cumulative, meaning each new dose can feel a little worse than the last, and this had been the case with me. The burning hands and indigestion were notably worse.
With the cancellation of round 12 settled, I was eager to ask some questions about my research. First, I wanted to know if the metastasis in my retroperitoneum was considered regional or distant. I was proud of myself for learning how to pronounce “retroperitoneum”, but then forgot how to say it there in the office. As I struggled to get it out, he made no attempt to help me. So I started laughing and gave up, jumping ahead to the question part: is it considered distant or regional?
He responded, “It depends. If it’s very far removed from the original tumor, it’s considered distant.”
I said, “Well, the sigmoid colon seems to be close to the retroperitoneum…”
He said, “It is, the only issue in your case is that it is not resectable. That’s what I meant before by ‘semantics’ – whether it is stage 3 or stage 4, the treatment is the same.”
So we moved on. Some of my other questions were:
- “Do we have a date for my Pet scan prior to surgery?” He said he would order it that day.
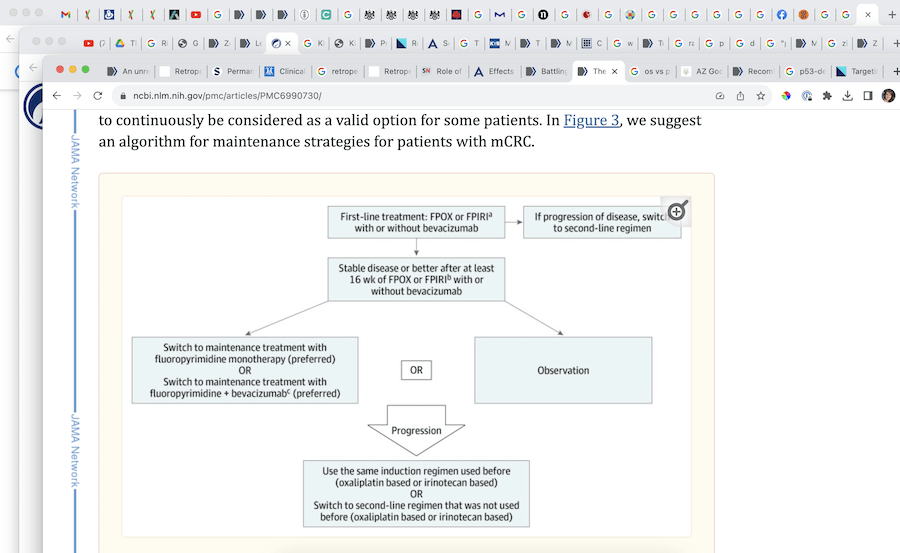
- “After surgery, regarding low dose maintenance chemo vs observation, the studies show that for my case, the chemo delayed PFS (time to disease progression), but had no effect on OS (5-year survival). My concern is about developing a resistance if I stay on the drug. If we do intermittent (observation) instead, and it returns, wouldn’t it be more likely to respond if we bring back what we knew worked the first time?” He said we’d likely go to something stronger either way, but added, “That’s a good question, I would prefer to do some sort of maintenance plan, but if your next scan and the operative findings are very encouraging, we could consider stopping and watching you.”
That would be ideal. I would love to take time after surgery to just work on rebuilding my health. But to feel comfortable with that, I have more research to do. While in January I felt like I was supposed to just go with whatever the doctor recommended, I have more recently started to feel that it is time (and that I finally have the capacity now) to take on the responsibility of knowing, not just what’s going on, but what I should be doing next.
After that visit with my doctor, we were off to the infusion room for my last foreseeable round, and we were on our way home.
Round 11 infusion complete, and going home with my pump.
____________
The first day of chemo is always relatively uneventful, but it does interrupt my sleep pattern. I’m usually wired into the night on the first day. That night, something on my mind was…
The Power of Prayer and Access to Heaven’s Blessings
… because just 11 days earlier, my sweet niece had been hit by a car after losing control of her bike in some dirt along a highway. The truck swerved to miss her, but the side mirror hit her in the head.
It wasn’t looking good, but the outpouring of love and prayers from friends, family, and community was massive. Her recovery turned out to be much faster than expected, and while we’re still waiting for her broken arm to heal, and praying she will regain sight in her right eye, overall, she’s been bouncing back in a miraculous way.
So, I was thinking about all the prayers that have been offered on my behalf and hers, and how much of a difference it has made for both of us. It left me wondering:
What if someone who really needs support doesn’t have an army of people praying for them, or putting their name on the temple prayer rolls? How is it fair for some people to have a lot of friends and family aware and praying, but not others? What about people who are alone, or who suffer in silence? Shouldn’t they enjoy the same kind of heavenly support, even if there aren’t a ton of people praying for them?
At 2am the words flowed into my mind accompanied by peace, so I grabbed my phone to create a note:
“They have their army on the other side of the veil. Nobody is without it. The prayers and faith we exercise on this side is for US, for OUR learning and growth, to learn how to connect with Heaven and participate in miracles.”
The thought felt true and comforting, and it reminded me of this:
“Fear not: for they that be with us are more than they that be with them. And Elisha prayed, and said, Lord, I pray thee, open his eyes, that he may see. And the Lord opened the eyes of the young man; and he saw: and, behold, the mountain was full of horses and chariots of fire round about Elisha” (2 Kings 6:16-17).
“In the gospel of Jesus Christ you have help from both sides of the veil, and you must never forget that. When disappointment and discouragement strike–and they will–you remember and never forget that if our eyes could be opened we would see horses and chariots of fire as far as the eye can see riding at reckless speed to come to our protection. They will always be there, these armies of heaven, in defense of Abraham’s seed.” ― Jeffrey R. Holland, Created for Greater Things
Setting my Intention – August 17, 2023
On day 4 of this round of chemo, I decided it was time to set another official intention of what I needed / wanted for feeling confident in my decisions about treatment after surgery. (BTW there’s a backstory to why I do this journal thing and how it works on this podcast episode.)
So I pulled up a new note and wrote:
What I needed / wanted 8/17/2023:
I would love to feel educated, knowledgeable, and confident in the path we’ve chosen for my health post-surgery. I’m grateful that the Lord guided me to have the right questions and find the right answers for my best, highest good.
I do believe that the Lord wants me to be restored to health. I believe there is a way to receive that blessing, despite the odds, as I discover what He would have me do. I pray that the way will be clear, and that I may have the capacity and motivation to follow it.
I’m grateful that I was given the clarity of mind to compile and present a sound and educated case for the path we’ve chosen, and that the doctor feels at peace with it as well. His continued support is so appreciated.
I choose to believe that God is going to tell a beautiful, edifying and inspiring story through my experience, and that it will help many of his children have greater success in their health goals, and that they will come closer to him through their own experiences.
Most of all, it is my request that I will feel confident and at peace with the decision we’ll make, and ready to present it to the doctor at my next follow-up visit after surgery.
With this intention established, I started getting ready for our trip to Utah / Idaho, where I planned to continue my research. I thought I’d have plenty of time to study things out and determine with confidence my next treatment plan.
As far as side effects for Round 11:
- Swollen uvula, burning fingertips (no Avastin this time so I was surprised at these side effects)
- Peeling feet and numb fingers
- Some acid reflux / belching
- Headache and queasiness on day 5
Taking Nicholas to college – Saturday, August 19. 2023
At the end of the week, we packed up a rented travel trailer to take our son Nicholas to BYU in Provo, Utah. We decided to turn it into a ‘visit family’ tour. Our first stop would be Boise to see my folks, Twin Falls to let Nicholas visit one of his old mission areas, Rexburg to see our oldest sons, Pocatello to visit another mission area, Salt Lake City to see our daughter and extended family, and then Lehi to see my sister and another son.
Originally we planned to drive straight up through Nevada to get to Boise (a route we’ve never taken before), just to make the trip more interesting. But at the very last minute, Hurricane Hilary was looking sketchy and pointed straight up the same path at the same time we’d be driving it. While it sounded adventurous to take the route in our Jeep anyway, the fact that we were pulling a rented trailer changed our mind.
So up through Kanab and over to the I-15 we went.
By the time we were an hour outside of Utah valley, our son Nathan called to ask what we were doing. Turns out he and Jacob were just rolling into Utah valley from Idaho themselves. We met them in a Provo Walmart parking lot and enjoyed dinner together in the trailer.
Thanks to the Hurricane Hilary detour, that time with our boys turned out to be really good for the soul, even though we’d see them again in Idaho a few days later.
Here we are in Rexburg, Idaho chillin’ at the park:
Pizza/Salad buffet at Pizza Pie Cafe, Rexburg:
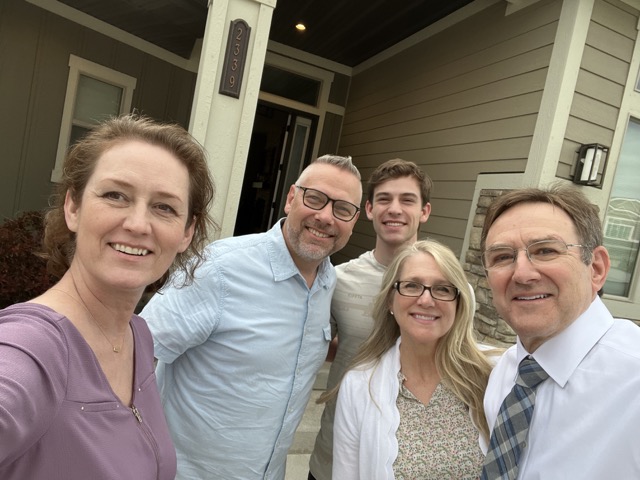
Meeting one of Nicholas’ former mission presidents and his wife in Pocatello. Nicholas served in Idaho while he waited for the Covid restrictions to be lifted so he could finish in Barbados.
My cute niece in SLC, Utah:
Trevan’s brother and wife (these Householder men and redheads…)
At Chick-fil-a, Saratoga Springs, Utah:
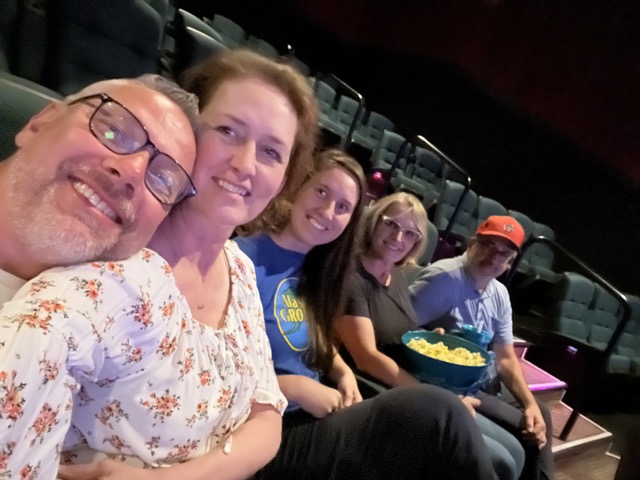
Movie night with our daughter, my sister, and brother-in-law:
Parking the little rented rig at my sister’s in Lehi:
Stopping for a Sacrament service before heading south:
Stopping at the sand caves near Kanab, Utah. It took too long for us to find the path up to the caves, and actually turned out to be too hot and too difficult for me to make the climb, so we found some shade for a quick picture and turned around:
Between Page and Flagstaff at the crest of the mesa:
Stopped for a night in Flagstaff:
This was the first day I really dug into my research because until this point, I’d just been having too much fun being with some of my favorite people.
It’s all so confusing!
We decided to take a gondola trip at the nearby ski resort before heading home:
A very important landmark:
Heading out for the last leg of our journey, on Route 66:
A couple days after we got home, I sent a message to my doctor.
Questions – August 29, 2023
- Is it okay for me to visit my dentist for a cleaning / treatment? I’m overdue and think I may have a cavity.
- I would like to improve my health/strength in preparation for the surgery Sept 19th (and possibly beyond if we opt for a period of observation). Is there an integrative oncologist or nutritionist you might recommend we add to my team? I’m just researching options so I can be prepared to make a fully informed / educated decision post-surgery. Thank you!
His reply: “You should be okay to get dental cleaning. Let me know if you need an extraction. We may need to check your blood counts before the procedure. I am putting in a referral for our Integrative medicine department and they can see you.”
I was thrilled to have his help in adding someone new to the team. I felt like getting a second opinion would be important for helping me gain the education I need to make the impending decision about treatment after surgery.
Observation: A Valid Option
In my studies, it appeared that in my circumstances, a period of observation without chemotherapy would be scientifically / clinically valid, as long as my next scan and the findings during surgery looked good.
“When compared with observation, maintenance therapy conferred a PFS benefit (HR = 0.58; 95% CI, 0.43-0.77) but no OS benefit (HR = 0.91; 95% CI, 0.83-1.01).” https://www.healio.com/news/hematology-oncology/20191219/switch-to-maintenance-therapy-appropriate-and-beneficial-in-metastatic-colorectal-cancer
“Although a maintenance strategy with a fluoropyrimidine with or without bevacizumab is preferred over continuous induction therapy for metastatic colorectal cancer, shared decision-making should include observation as an acceptable option, given the lack of significant overall survival benefits.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6990730/
“It is generally accepted … that patients with complete clinical responses may discontinue chemotherapy until radiographic evidence of disease recurrence emerges. Although the overwhelming evidence supports the use of chemotherapy in metastatic CRC, a subpopulation with indolent disease probably exists, where observation may not be unreasonable.” https://ar.iiarjournals.org/content/29/2/465
After all, low-dose 5FU by itself (maintenance therapy), would be a gamble due to my tp53 mutation:
Several in vitro, animal and clinical studies have shown that normal p53 is required for the response of colorectal cancers to 5-fluorouracil-based chemotherapy. https://pubmed.ncbi.nlm.nih.gov/12619112/
If my upcoming scan shows the disease had grown or spread, then of course observation only would probably be foolish. I was still feeling like the spot was gone, so I looked forward to the results so we could confirm whether it was really the case.
PET Scan Denied
About this time, I was notified that my insurance had denied PET scan approval, since already had one in June. The request was appealed, but denied again. My doctor fought it, and the decision was ultimately reversed a few weeks later.
Pain in the Neck – September 6, 2023
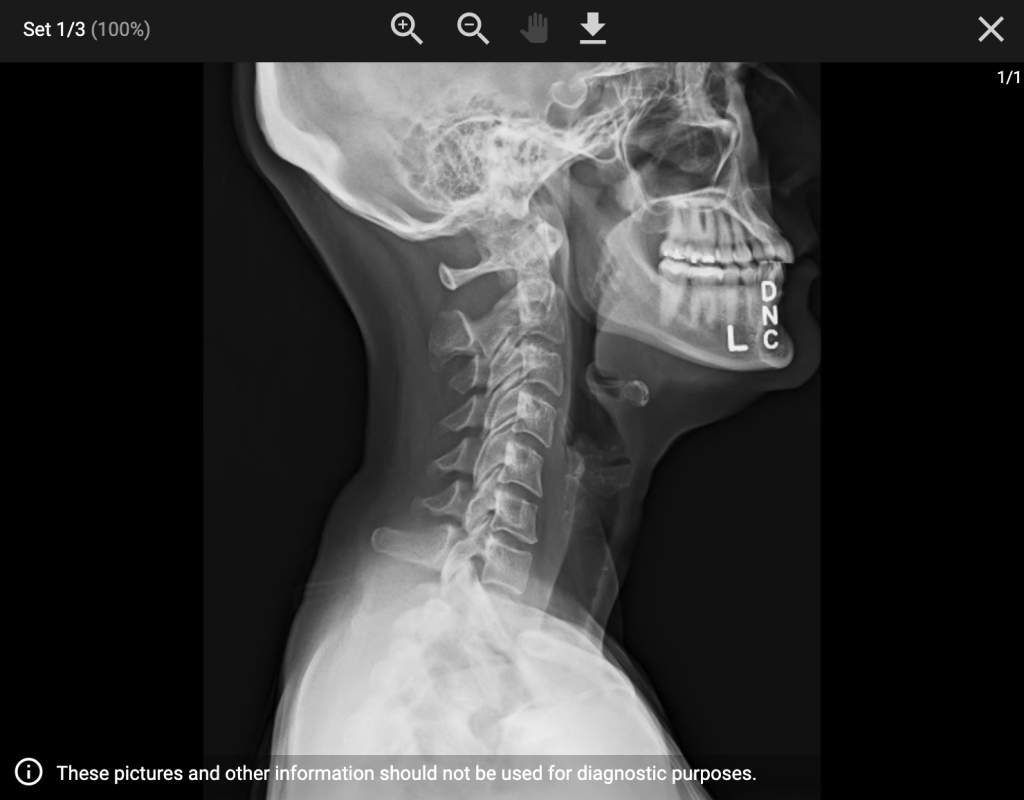
Before leaving for Utah, my neck was feeling kinked. I just dealt with it, hoping the pain would go away on its own. Weeks later, I was still battling it, and it was getting worse, causing some brutal headaches. I avoid chiropractors and myopractors until I can’t take it anymore and then I eventually submit. But I had a thought that maybe I should run it past my oncologist first to make sure there wasn’t some reason I shouldn’t. He said he didn’t want me to get an adjustment without first getting a CT scan, so I cancelled my appointment and went in for the scan.
Thankfully, nothing was found on that scan.
Too much of a good thing isn’t good – #overthinking
Back to my research… As much as I would love to believe there will be an endpoint for all there is to learn, I find myself going down endless rabbit holes of data with very little definitive information to offer me solid right answers about what I should be doing from science alone. I keep thinking I’m almost to that breakthrough – to the piece that ties it all together, wrapped up in a beautiful bow. But every time I think I’m nearly there, I stumble onto some new information that refutes a previous conclusion.
For example, I’ve been thinking for weeks that the p51 gene could take over for my faulty TP53, but just today I stumbled onto the report that said p51 isn’t “everywhere” in the same way p53 is. It’s found in several other tissues, just not the ones that matter for me.
Information Overload and the SQUEEZE
The data has all just become too much. I can’t seem to get it organized, despite the hundreds of hours I’ve spent.
I’ve been too much in the weeds of it – with 40-90 tabs open at a time, a giant encyclopedia of integrative oncology at my side, and a raw DNA report crashing my system, just from trying to copy/paste it into a spreadsheet.
As we say in Genius Bootcamp, I’ve been in the “squeeze” for too long.
My goal has been to feel educated, and I feel it! But I need to get to where I can make the necessary decisions and be totally at peace with them. Sometimes I can only get to that peace of mind after a good squeeze, when I finally “let go”.
As it is with sponges, sometimes the thing we want can only be drawn in after we’ve relaxed our grip.
I had a conversation with a member of the science board for Avini Health, the producer of the micronized zeolite, and I was reminded that the body does millions of things we don’t understand. Sometimes we have to exercise faith and trust in our divine design, and the inherent capabilities of our bodies. They were designed to heal, and I don’t have to understand every gene function or backup mechanism to determine my next right step.
I get that, but when I learned that I was lacking a gene that our immune system relies on to kill cancer cells naturally, I realized that it could have been a fatal decision to rely only on natural remedies to beat this thing. I’m reminded of the moment I heard my diagnosis and felt a calm but assuring sense that I needed to submit to whatever the doctors wanted to do for me. Fast forward 9 months, and I feel a similarly calm but assuring sense that it’s time for me now to prepare to make my own recommendations for treatment post-surgery.
It makes me think of The Jackrabbit Factor which tells a story about a man on a road trip with his family, where something inside told him to make sure everyone was belted up. As they rounded a corner, they had a head on collision. When he related the story later to his friend he said, “Those seatbelts saved our lives!” His friend replied, “No, the seatbelts didn’t save your life; whatever told you to put them on saved your life.”
It’s not what we DO that matters as much as the WHY we do it.
That’s a principle I’ve been trying to live on my journey to health. To pay attention to the nudges that help me know my next right step, and not just what to do, but WHEN to do it. Clearly, I needed chemo in the beginning. I’m not so sure I still need it now.
That’s why I’ve been doing all I can to gain the education I need to make a sound decision, but there truly comes a point when it’s time to just make the best decision you can, even if you haven’t been able to come to a definitive, fail-proof conclusion. Maybe in this case there isn’t one, and I’ll just have to take that leap of faith.
Running out of Steam
Anyway, time was running out and I was running out of steam. As if researching cancer treatments weren’t overwhelming enough, I was also needing to decide how much of my UroGyn’s proposed procedures I would have her do during my surgery Tuesday. There is SO much to figure out. But this quote helped a lot:
Sunday School – September 3, 2023
“What may appear initially to be a daunting task will be much easier to manage over time as you consistently strive to recognize and follow feelings prompted by the Spirit. Your confidence in the direction you receive from the Holy Ghost will also become stronger.
“I witness that as you gain experience and success in being guided by the Spirit, your confidence in the impressions you feel can become more certain than your dependence on what you see or hear.
“Spirituality yields two fruits. The first is inspiration to know what to do. The second is power, or the capacity to do it. These two capacities come together. That’s why Nephi could say, ‘I will go and do the things which the Lord hath commanded.’ He knew the spiritual laws upon which inspiration and power are based. Yes, God answers prayer and gives us spiritual direction when we live obediently and exercise the required faith in Him.” – Richard G. Scott
That’s what I need. I need to feel more certain about the guidance from the Spirit of God than I feel about what I’m reading. Actually, when put that way, it doesn’t seem so hard. The Spirit guides us subtly, calmly. The scientific study I’ve engaged in has felt so much more frenzied. Necessary, I think, to come to the best conclusion I can, but how sweet it will be to take the decision to the Lord and see if I can feel whether he ratifies it.
Biopsy Report – Wednesday, September 6, 2023
The tissue sample from my colonoscopy was benign – yay!
This was also the day a phlebotomist came to take my blood for my second Natera ctDNA test, which looks for whether any cancer cells have sloughed off into the blood stream – an early indicator of the likelihood of the cancer spreading to distant organs. The results of my first test three months ago showed zero cancer cells in my blood. We’re hoping this one will be the same, but I don’t have those results back yet.
I also went to see someone about my neck pain. Nothing I tried was helping. Not the recommended pain medication, nor adjustments (which usually do the trick). So I started using ice packs and ordered a neck brace to give me some traction. The neck brace arrived today but isn’t doing what I hoped, so it’s getting returned and I’ve ordered a different stretching device that should be here tomorrow.
Friday, September 8, 2023 – pre-op with UroGyn
We discussed everything she will be doing on September 19th, and if I wasn’t already overwhelmed before this appointment, I certainly was afterward. Only because I have between now and then to decide whether to have her to everything, or only some of it. It’s a lot, and recovery will be challenge. How much do I really want to be recovering from? Will the benefits outweigh the risks? Yet another thing to research, with conflicting reports to sort through.
Monday, September 11, 2023 – pre-op with GI Surgeon
Since the doctors will be putting me under and taking turns doing their part, I had to meet with both of them to discuss the procedures. This appointment with my GI doctor changed everything.
I think the quickest way to explain what happened here is to share part of the convo I had with my family about it:
Tuesday, September 12th
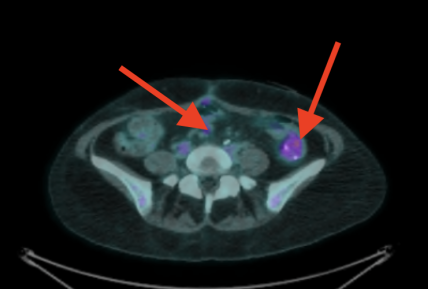
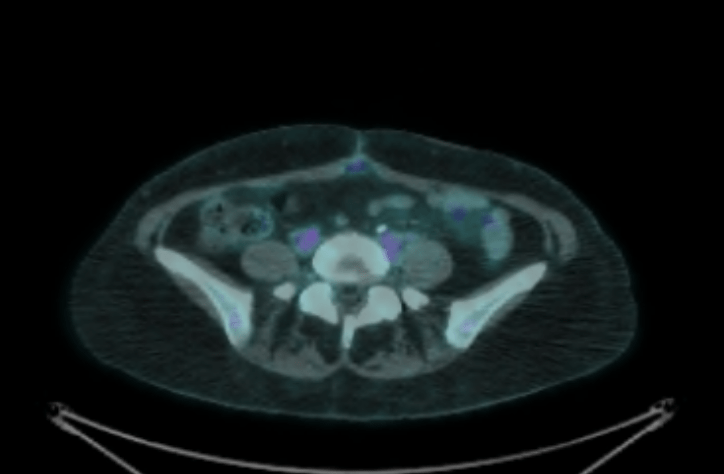
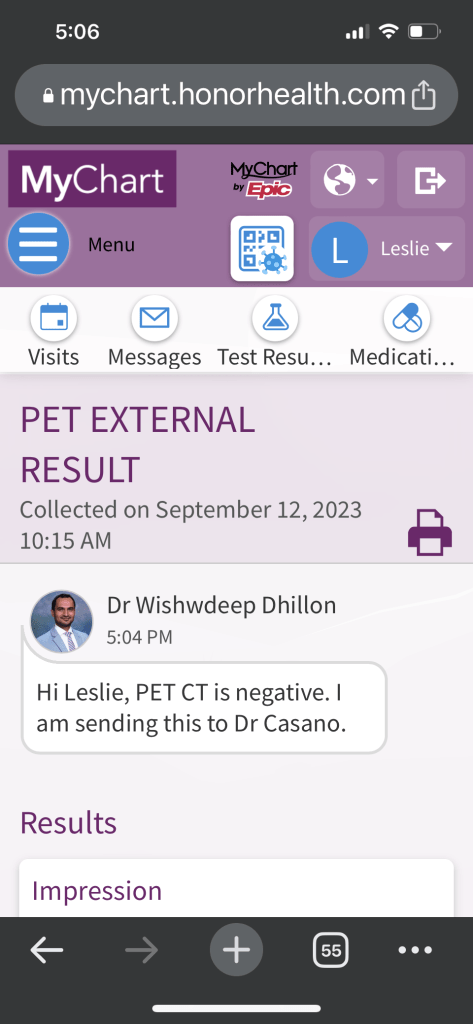
Hey family, I had my PET scan this morning. It usually takes 2 days to get the results back, but I got a message less than 2 hours later that my results had been posted.
It had a lot to say, lots of jargon. It said the spot we’ve been working on has not shrunk, so that’s a bummer, but it also said it is no longer considered malignant. Nothing lit up as cancerous. So that’s really good news! I won’t feel like it’s entirely over until I can keep my scans clean for the next 4.5 years, but this is a good start.
I also met with my surgeon yesterday to ask some questions about my upcoming surgery next Tuesday. One thing I should probably update you about, is I asked her, “with me being stage 4, were you surprised to see no other polyps on the colonoscopy?” and she came back quick with, essentially, “Let me correct you – you are NOT stage 4. You are stage 3.”
(Now, my oncologist has been treating my tumor like it’s a distant metastases, which I translated to mean stage 4. So, because of the way I understood it, pretty much all my research has been based on that understanding. Here my GI surgeon is setting the record straight.)
I responded to my son:
So basically much of the 24 pages of notes and links I’ve been gathering may not even be relevant. I mean, I’ve enjoyed the study; never have I ever geeked out so much about biology, but I feel like I need to start over. Not really. I just need to sift through it all again and see what it all means to me with this new paradigm.
Anyway, I’ve been apprehensive about my surgery Tuesday. They are doing a lot of things that will be uncomfortable through recovery. Lots of reconstructing things, pelvic floor repair, hysterectomy, ostomy reversal… about 6 different procedures all at the same time and it just feels like a lot. Recovery time is expected to be about 6 weeks to 2 months.
There are two procedures that I have until Tuesday to decide whether to have them or not. I could use your prayers from now until I recover, to help me make the right decisions in what all I should have them do, that the surgery will be completed without complications, that I will be strengthened in my recovery and that I will bounce back swiftly. Will you guys support me in this?
My son:
Of course we will! Thanks for the update mom. How are you feeling about things in the moment?
Me:
I should be feeling really happy but I’m in this weird place with the surgeon’s comments because it’s making me question what’s real, and how much of my experience the last couple months was what it was because I was operating from a misunderstanding. I feel a little – shell shocked isn’t the right word – stunned? No – taken for a ride? Not sure – hard to describe. Reeling? Mostly because I’ve spent probably a hundred hours poring over medical journals, learning really hard stuff, new vocabulary … cross referencing everything…. about the wrong thing.
My son:
Ah yeah that totally makes sense. I’m sorry! Is the ‘experience’ that different between the stages? I understand that what they mean is different, but what about the experience of it?
Me:
I’m not mad… just … ugh can’t find the right word.
My son:
Disoriented or bewildered?
Me:
YES! Bewildered is perfect.
Well, stage 4 historically has been a terminal diagnosis, incurable. In recent years it hasn’t been as much of a death sentence, but life feels different when you think odds are not in your favor.
…Stage 4 means it’s spread distantly to other organs and the rest of your life can be expected to be a game of whack a mole, hoping to kick each new spot before it kills you. Stage 3 is where it’s only spread to some regional (nearby) lymph nodes. Prognosis is much better. Still serious, but odds are definitely higher for a complete recovery.
The confusion in my case happened because mine did spread, but only to some nearby lymph nodes, one of which was inoperable. That’s the one we’ve been working on shrinking. It basically sits on a major vein, so the surgeon didn’t dare cut it out.
My oncologist has been calling it a metastasis, which generally means it’s spread to a distant site. But according to my GI surgeon, it’s not a metastasis. Technically it would have to show up on something like the liver or lung to be called that.
As far as the “experience” – the chemo treatment would have been the same. It’s what goes on in your head that is different. That is, until the Stage 4 cancer starts affecting other organs, then I’m sure it would physically feel different, too.
My son:
Oh dang yeah that makes sense. Btw ChatGPT gave me “bewildered” 😂. I’m sorry you had to go through all of that mentally 😢. Although you aren’t sure how to feel right now, do you see a hope for the mentality shift in the future?
Me:
Yeah, I just need to let the news settle. Meanwhile feeling anxious about the surgery. I can see the light at the end of the tunnel maybe around mid October.
My daughter:
Could it turn into stage 4 or do the stages stay kinda the same?
Me:
It could turn into stage 4, which is why they will be monitoring me for a total of 5 years. After that, if there haven’t been any recurrences, I’d be considered in the clear.
My daughter:
Wow that is so much
My son:
You said that the spot they’ve been focusing on hasn’t really shrunk, but I thought that each scan looked like it was shrinking? To the point we couldn’t really notice it?
Me:
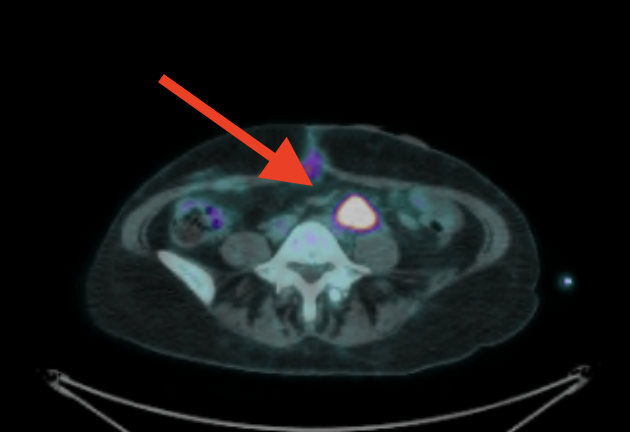
I’ve had 3 scans. First scan it was 3cm with a SUV max score of 5 point something. (For my type of cancer, 2.5 or above is considered cancerous… it’s how much of the radioactive stuff is detected in the spot. Or something like that.) My second scan it was about 1 cm with a SUV max score of I think 2.6. Then this last scan it was still 1 cm but the SUV max score was 1.9. I’d have to log back in to confirm those numbers but that’s what I recall.
After that conversation I wanted to dig up my original diagnosis from January and figure out how much of my research was based on the (perhaps) misguided evolution of my understanding, and not even relevant. What really IS my prognosis? Not that it should matter, but if I do beat this, I would love to understand how miraculous it really was.
I found the note in my original surgery report: pT4b, pN1b, Mn/a.
- pT4b means the Tumor has grown through the bowel wall into other organs. In my case, it spread into one spot in the small intestine, which they resected in January.
- pN1b means there were 2-3 lymph nodes involved. In my case, there were 3 out of 20 found to have cancer. This was later verbally updated to pN2a which means at least 4 nodes were involved. In my case, the 4th node wasn’t originally counted because it was left un-resected on a major vein.
- Mn/a means there is no metastasis – no spreading to distant organs.
In defense of my oncologist who has been calling my lymph node a metastasis, I’ve been finding just as many articles that call lymph node involvement just that, even when it’s not stage 4. Conclusion: Although my doctors disagree on this point, I can see now why they are both justified in their points of view.
Before understanding how they can both be right, those disagreements had left me feeling confused, as my prognosis seemed to be changing weekly depending on what I read, or what I heard my doctors say. Now that I’ve found my original TNM score, I guess you could say my actual prognosis would be derived from this:
The 5-year relative survival rate for T4 colon cancer varies from 79.6 (T4a) or 58.4% (T4b) in case of no lymph node involvement (N0), to 40.9-54% in case of nodal involvement for T4a category, but significantly lower for T4b category with nodal involvement (15.7 – 38.5%) [6,7,44]. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6295185/
A survival rate of 15-38% is much more grim than the Regional 72% I thought it was. Yes mine is regional, but the T score definitely changes things.
Friday, September 15, 2023
I’ve been off chemo now for more than 4 weeks and goodness gracious, my feet are still burning and peeling. It’s cooler outside now, so my husband and I have starting walking at night. I can go pretty fast now and I’m not getting fatigued like I’ve been most of the year!
Last night I revisited all the decisions I’ve been feeling pressured to make, and feeling torn between them even still, I figured I might make some progress if I would just decide. I made a list of what I was deciding to do, and felt pretty comfortable with it. The next day, I felt absolutely the opposite. When I asked the Lord in prayer for some clarity, I got one of those “it doesn’t really matter” kind of responses.
So, no, I’m still not fully decided. But I’m feeling less stressed that there is too much at stake to get it wrong.
It Hasn’t Sunk In
Man, can you hear/see my thoughts just spinning?
All that spinning, and yet somewhere in the middle of this update I got a clean scan. I got a clean scan!! But I don’t even feel like celebrating. I’ve tried telling a few people here and there to see if I could generate the thrill you’d think a person in my situation should be feeling, but really don’t feel particularly thrilled.
I think there may be a few reasons for this. Because:
- I already lived the thrill in my head back in April. Since I’ve already been feeling like it’s gone for a few months now, there was really no delta to be experienced in my emotions. The news really didn’t change how I felt except to confirm what I was already feeling. So, not a “thrill”; just more like a “check-the-box” kind of thing.
- Even though my CEA, ctDNA, and PET scan ALL show no signs of cancer right now, it’s not considered complete remission until you get to 5 years without recurrence. Maybe it just feels too soon to celebrate?
- I’m still feeling bewildered that I invested so much energy into researching the wrong information. Maybe it’s still relevant, maybe not. I haven’t had the energy or desire to go back and fully figure that out yet. Nor may I ever. I’m thinking maybe I shouldn’t even try. Or at least I should let it rest for a bit before I go after it again.
- On the heels of this good news, I’m heading into a really big surgery on Tuesday (Sept 19) that has me a little worried. I need to do some mindset work on this one.
- I saw the scan, and frankly the spot looked no different to me. Yes, the SUV max score was down into the normal range for the first time… but that spot. I questioned my surgeon about it, and she encouraged me to stop overthinking and just let it be the good news that it is. I’m telling myself now, BREATHE Leslie, for crying out loud, breathe already.
February: 3 cm:
June: 1 cm with inflammation at the staple line of my Hartmann’s pouch:
September: Inflammation resolved, spot still 1 cm (but no FDG uptake):
But despite my hesitation to celebrate…
I’m cancer free.
There you have it. I’m certainly not announcing it the way I planned. But here we are.
I didn’t even get the results in the way I thought I would. I think I had pictured seeing the word “NED (No evidence of disease)” on the scan report. Instead, it said a whole lot of extra things, even reporting on some non-cancerous problems I didn’t even know I had. Specifically:
No FDG avid disease in the neck. (I had asked them to look because of the pain I’ve been having there.)
No FDG avid thoracic lymphadenopathy. Tracer activity along the course of the esophagus is consistent with inflammation. Mild biapical scarring. Right upper lobe nodule (image 98) is stable and not FDG avid. No FDG avid pulmonary lesions.
Previously depicted left retroperitoneal nodal mass in the common iliac station measures 0.9 cm in short axis, unchanged (SUV max 1.9, previously 2.6, image 224). Elsewhere below the diaphragm, tracer activity is unremarkable. Calcified mass closely associated with bowel in the left hemiabdomen is unchanged. Left renal cyst. There are postoperative changes of the colon with left lower quadrant ostomy. There are no FDG avid skeletal lesions.
No findings convincing for FDG avid malignancy. The left common iliac nodal lesion is not FDG avid and is similar in size to the prior study.
Anyway, do you feel me?
Does this look like the kind of “clean scan” report YOU would have envisioned? Me neither. My oncologist’s summary was much simpler, but still not quite what I had imagined:
I’m trying to let myself feel grateful, and to soak in the joy of it. It really is awesome news!! And maybe with next week’s surgery behind me I’ll find it easier to relax into gratitude. I can hope so.
Anyway, if there’s any lesson to be learned from the last 4 weeks, I think maybe it’s that I just need to do better about challenging my assumptions so I don’t spend so much energy chasing distractions.
So that’s pretty much it. If you’ve read this whole thing, I think you should get a trophy. I’ll try to do better about posting updates more often so they don’t have to be so long.
Thank you for your prayers, they’ve been working.
This week, I could really use your prayers on the following:
- To help me make the right decision about which of the procedures I should have my surgeons do or not do
- that they and the hospital staff will be inspired, guided, and supported as they work on me
- that the surgery will go smoothly and successfully
- that I will be strengthened in my recovery, and
- that I will bounce back swiftly. Because…
(this is a PS) I’ve been working on an article since April that will outline the distinctions between Rare Faith and New Age philosophies. Where I thought they were similar, the differences are turning out to be pretty vast. It’s been on my mind a lot, and thinking about it sometimes keeps me up at night. That’s one reason why I want to recover quickly. I need to finish that article!
Anyway, keep your eye out for it, I’ll be posting it sometime after my September 19th first class trip to Chandler Regional.
- New England’s Dark Day - July 6, 2024
- Something was missing - June 17, 2024
- A goal to find a goal - June 14, 2024






































6 Responses
You’re in our thoughts and prayers today Leslie!
Visualize your life like it has been 5 years and you are clear. Take all your wins and rejoice. Please stop eating processed foods and sugar. Stick to as many greens in the produce section as you can. Avoid feeding any remaining cells with sugar (including sweet fruits). You can do so much to fight for yourself. You are cherished by so many. Keep fighting. Keep imagineering.
I, along with so many others, have followed your story all along the way. We love reading your thoughts articulated into words. We love sharing your experience with you and are drawn to you and your wisdom. Continued prayers for your energy and ALL that you desire. We are sure you will know and do what is right for you, and that you will continue to inspire and encourage us to be our “best-and-getting-better” selves! Love and hugs!
I appreciate this, Lana!
WOW! My brain never wants to attempt to wade through technical stuff, but I read that entire post to get to the “punch line” – I’m cancer free. That right there is enough for me to get excited about!! WITH YOU. Of all the stuff you’ve been through, I can relate most of all with colonoscopy pre-cleaning. I had to have part of my colon removed several years ago, which leaves me taking those things regularly. I’ve never made it all the way through drinking the stuff-it’s definitely the worst. But who cares about all of that, I’m so happy to read “I’m cancer free.” I definitely rejoice with you and your family and friends for every single win you have.
Lord God, I am incredibly blessed and optimistic for Leslies future and knowing that her health is being restored. I join her and many many others in thanking for your incredible blessing on her life here on earth. I ask you in Jesus name that you continue to watch over, protect her, and guide into making every right decision and making sure they coincide exactly with your personal will and leading for Leslie Householder.
Thank you Mike!